CHRONIC PAIN: what, why, how AND WHAT you can do about it
Part 2 in understanding how your body interprets pain
Written by Resilient Health Osteopath Dr Mel Pierlot.
Chronic pain refers to pain that lasts for more than 3 months or past normal tissue healing time. The development of chronic pain is complex process, but understanding how and why chronic pain happens will give you the power to manage it.
Chronic pain is not a symptom, but is a disease in its own right, associated with:
- Disturbed sleep
- Depression
- Irritability
- Decreased activity level
- Social isolation
If you haven’t already, please read the first blog on acute pain:
https://www.resilienthealth.co/blog/62-what-is-acute-pain-the-basics-of-pain-science
In the last blog we learned that:
- Pain is an interpretation that the brain makes, but pain is still very real
- We will feel pain well before there is any damage to protect us
- Pain involves many parts of the brain, including the memory, learning and emotional centres of our brain
What is chronic pain?
Here is a picture of how acute pain works in the body. It demonstrates how we feel pain before there is any damage to the tissues in our body.
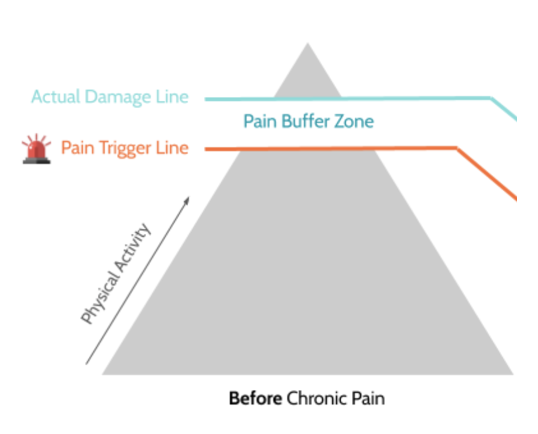
Then we compare it to what chronic pain looks like:
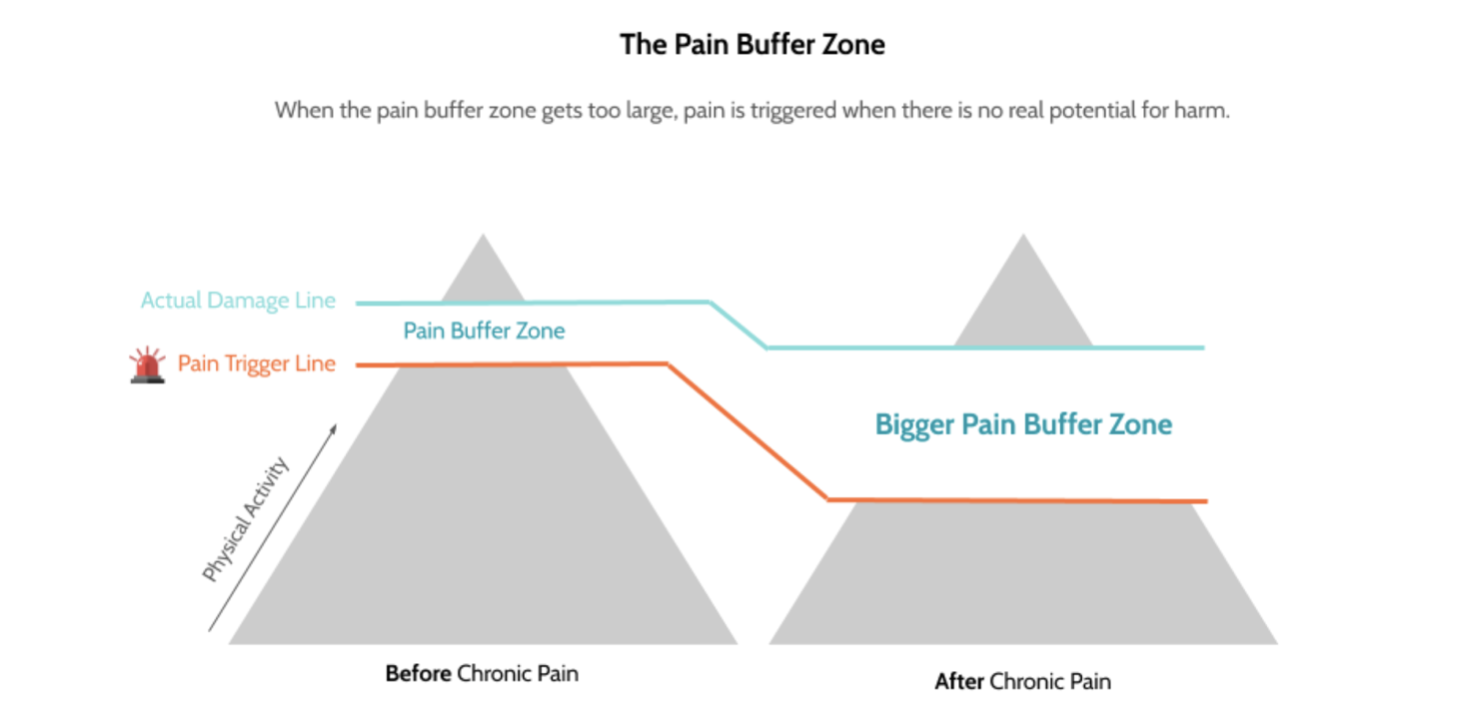
What we can see from the chronic pain picture is that in a chronic pain state it is easier to feel pain. Our pain system becomes overprotective. This process, this widening of the buffer, is our pain system becoming more sensitive.
Chronic pain is essentially the sensitisation and overprotection of our pain systems, after the injury is healed.
Why does it occur?
So what makes our pain system to become sensitive and overprotective? It’s complicated.
We know that pain is designed to protect us. So anything that our brain believes could harm us, has the capacity to prolong or increase our pain.
Because pain is formed using many different parts of the brain, our pain system can be triggered by more than just tissue stress. Harms or threats may be physical, emotional, social, or psychological. In chronic pain it isn’t just about the injured body part; anything that overwhelms our body systems or threatens you as a person becomes capable of creating pain.
This means things like the sight of your stack of work on your desk, depression, anxiety, personal beliefs and poor self esteem all have the capacity to produce pain, just as much as heavy lifting or straining can. Remember that thoughts, feelings, learning, memory, people, places are all nerve signals too.
How does it occur?
Sensitisation of the pain system is a complex process and it occurs in our tissues, brain and spinal cord. Without getting too technical, essentially what happens is:
1. Our nervous and immune system become more sensitive.
The threshold that is normally required for our pain system be activated is reduced, so things that normally wouldn’t be painful, become painful.
2. Our nerves develop stronger and broader connections with each other the more we activate the pain pathway
“Nerves that fire together, wire together”.
3. There are physical, structural changes in your brain and spinal cord that make your system overprotective and oversensitive
Collectively, this process means that your brain is receiving information that no longer reflects the true state or health of the tissues that are painful. And the longer this process goes on, the better our system gets at producing pain.
How do we OVERCOME it?
Although this all might sound very bleak, an important take away is that in the same way that our body learns pain, it also has the extraordinary ability to unlearn it!
Because chronic pain occurs overtime and involves changes in many different tissues of the body, it is important to remember that recovery takes time and a long term approach is needed.
This diagram might help:
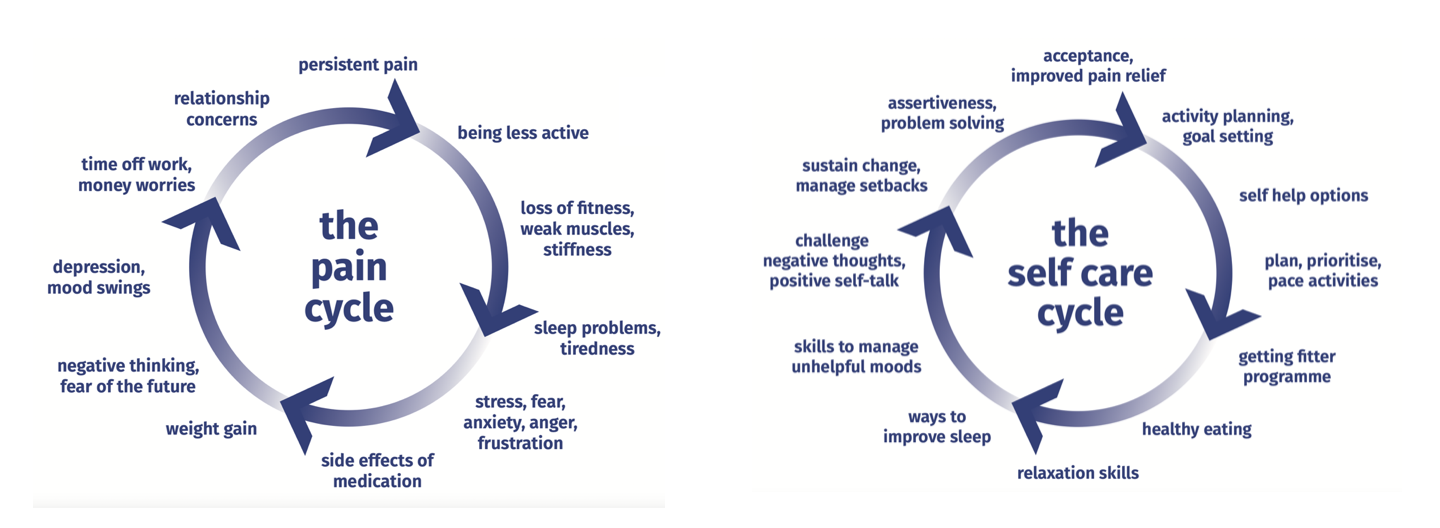
This is why your rehabilitaiton includes a variety of things. Especially:
Graded exposure exercise:
The sensitivity of our pain system can reduced by slowly challenging the system. By exercising and moving, your brain and system will learn that movement is safe and will subsequently send less pain signals. You need to increase your exercise/ movement enough to challenge the hardwiring of your system, but not too much that your system feels overwhelmed or triggered. Graded exposure exercise is best done with a healthcare professional who can guide you through this.
Pain psychology:
We know that chronic pain has a lot to do with our psychological and social environment, so speaking with a pain psychologist or specialist can help to manage any unhelpful beliefs or thoughts that may be feeding into the pain cycle. You can also start this process at home. Anytime you come across something that causes you pain, remind yourself:
- That your pain does not reflect the health of your tissues.
- Pain is a response that your brain conjures because it feels unsafe. Tell yourself that the activity you are doing is safe and that you are capable of it. Ask yourself why you might be feeling protective in that moment.
- Check in on your self esteem. Instead of saying ‘I can’t do this’, remind yourself that the body is resilient and that the body can learn. Thoughts and feelings are nerve signals too.
- Reduce stress. Find ways to integrate stress reduction in your life. It can be as simple as meditation, listening to music that makes you feel good, breathing exercises, journaling or grounding, improving sleep and diet. Anyways that we can reduce extra stress on our body will down regulate the sensitivity of our system as a whole.
See you in the clinic!
The Resilient Health Team
References
Brukner P, & Clarsen B, & Cook J, & Cools A, & Crossley K, & Hutchinson M, & McCrory P, & Bahr R, & Khan K(Eds.), (2017). Brukner & Khan’s Clinical Sports Medicine: Injuries, Volume 1, 5e. McGraw Hill.
International Association for the Study of Pain. (2020, July 16) IASP Announces Revised Definition of Pain. https://www.iasp-pain.org/publications/iasp-news/iasp-announces-revised-definition-of-pain/
Pain Revolution. (n.d.). The Key to Understanding Pain. https://www.painrevolution.org/factsheets
Yang, S., & Chang, M. C. (2019). Chronic Pain: Structural and Functional Changes in Brain Structures and Associated Negative Affective States. International journal of molecular sciences, 20(13), 3130. doi.org/10.3390/ijms20133130
IMAGES FROM:
https://www.hingehealth.com/blog/movement-is-medicine/
https://livewellwithpain.co.uk/resources/resources-for-your-patients/the-pain-cycle-visual-aid/
